Bioethics Forum Essay
Turning Lemons into Lemonade: Studying the Emotional Impact of Clinical Ethics Consultation
During my first year of graduate school, I was questioned by a professor because I arrived five minutes late to his seminar. Little did he know, I was in the midst of my first months on a clinical ethics consultation service and I had spent the preceding hour on the phone with two attending physicians, both of whom were deeply troubled by their roles in caring for a young patient on the brink of death. I had a choice. Curtail the call or be late for class. I opted to compromise my usual punctuality to finish the conversation. As I sat down in class, I said to myself, “if only he knew what was going on in the ‘real world’.” Needless to say, my mind was elsewhere during class that day.
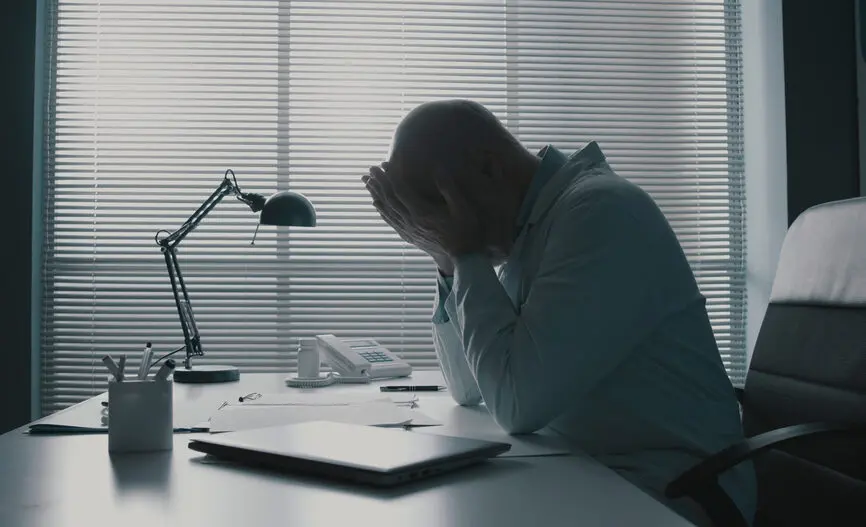
That moment of frustration was pivotal. It would go on to inform my dissertation, a chapter of which was recently published in AJOB Empirical Bioethics. My research centered on qualitative interviews with 34 clinical ethicists who were asked to reflect on the ways in which their work has impacted them emotionally. The interviews were raw, and the participants were vulnerable; they described cases that were troubling, agonizing, and harrowing. Some shed tears. Others lamented how frequently they felt helpless.
The stories participants shared with me were not unlike the case that resulted in my tardiness to class, which I’ve fictionalized here. The day before that seminar, we were consulted by a surgical attending regarding a critically ill patient with a complicated psychosocial situation who was going to require a very high-risk, life-altering surgery. The involved clinicians appeared uncertain about their roles and distressed about decisions they were confronting. I did my best to provide whatever support I could, but it was hard to be in the position of knowing that nothing I could say, or do, would objectively change the predicament they faced.
I was overwhelmed. Not only were the clinicians looking to the ethics service for guidance, but I identified with the patient, who was close to my age. She could not speak for herself and was either going to wake up in entirely different life circumstances or she was going to die. These facts circled my mind as I navigated life as a student. It all felt oddly disjointed; ethics in the classroom was a refuge largely disconnected from the life-and-death realities of ethics in practice.
As the case unfolded, a close mentor called me while she was making dinner. She was not the senior clinical ethicist on service, but had heard about the case and wanted to check in. Our conversation stands out in my memory because she was calling to see how I was doing. I had been so focused on the feelings of everyone else that I hadn’t paused to consider my own. But she did. It was the first time I cried over a case (though certainly not the last).
Those tears eventually brought a deep insight that helped to shape my career path. They were illustrative of a more general observation: While I anticipated the intellectual demand of clinical ethics consultations, I was far less prepared for the emotional weight that accompanies the work. When I checked the literature to see if others had made the same observation, I was further troubled by the fact that there were so few firsthand accounts of what it’s actually like to be a clinical ethicist. Complex Ethics Consultations: Cases That Haunt Us was probably the most direct acknowledgement of the challenges associated with the work (though it, too, largely framed ethics cases in an academic light). I began to question whether I was cut out for the work. Could I handle it? Was I too much of an empath? What if I didn’t want to feel this way for the rest of my career? Was I the only one struggling with the emotional side of the work?
At some point, it occurred to me that I could actually research the emotional burden of ethics cases on clinical ethicists. This was an epiphany. And, while existing literature on the topic was scarce, there was precedent in other, more established fields. Literature on the emotional experiences of other health care professionals, such as physicians, nurses, and social workers, had grown during and after the Covid-19 pandemic as their well-being gained attention.
After giving it some thought, I knew I had found my niche. I had to talk to clinical ethicists to learn about their experiences. I’m glad I did. My dissertation found that clinical ethicists do indeed appear to bear a significant emotional burden and that their professional experiences and coping mechanisms appear to be significantly influenced by the organizational structures around them.
Of course, in my capacity as a researcher (and a practitioner of clinical ethics) I knew I might have a bias. It was important to recognize the ways in which my ongoing experiences shaped the lens through which I viewed the data. But I largely regarded my inside status as a strength; as many of our participants shared, it is hard to understand the work unless or until you do it. To mitigate any personal distortions, however, I drew upon grounded theory because it required an awareness of my own position in relation to the research.
By bringing theory to practice, I hope that that my research will help clinical ethicists realize that they are not alone. It certainly helped me.
Anna D. Goff, PhD, HEC-C, is a medical ethics fellow at Weill Cornell Medicine LinkedIn: anna-d-goff
Acknowledgement:
I acknowledge Dr. Joseph J. Fins for encouraging me to tell my story in this forum. His input and feedback are greatly valued. I also thank Dr. Monica L. Gerrek for being the mentor that called me all those years ago. She created a space safe enough for a young trainee to voice her struggles. And, finally, I recognize my colleagues and mentors at both Weill Cornell Medicine and the MetroHealth System. It’s been a privilege to spend time at two institutions that offer such rich, supportive environments for learning.