Bioethics Forum Essay
Plan, Safeguard, Care: An Ethical Framework for Health Care Institutions Responding to Immigrant Enforcement Actions
There have been several recent efforts to outline the ethical duties of hospitals and other health care settings on how to respond to actions by Immigration and Customs Enforcement or other authorities concerning immigration enforcement in these settings. Here, we synthesize and build on those efforts, drawing on prior work by The Hastings Center, to create a practical ethical framework for health care institutions.
Key sources include “Health Care Institutions and Immigration Enforcement: An Ethical Imperative” by Julie M. Linton and colleagues, published in Health Affairs. Linton and co-authors draw on The Hastings Center’s Ethical Framework for Health Care Institutions Responding to Covid-19 (March 2020) to establish foundational duties for institutions that derive from their mission. Other sources include a commentary by bioethicist Mark Kuczewski. With these sources, we adapt The Hastings Center’s Covid-19 framework, which responded to the prospect of leading and working under conditions of stress and uncertainty during a public health emergency, for the situation now confronting health care institutions and their workforces in the United States.
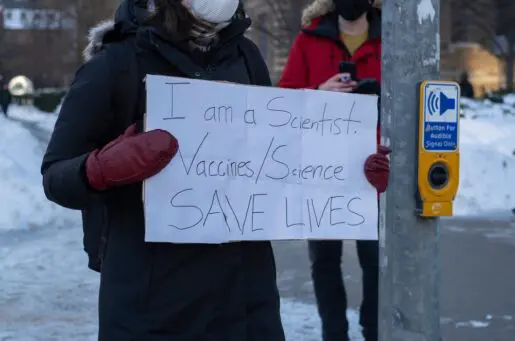
Health care institutions meet basic human needs by providing essential services that save lives, restore health, or manage symptoms of health conditions. In the U.S., access to health care services is frequently constrained by lack of insurance and by ability to pay. Yet every person, regardless of socioeconomic resources, citizenship, or immigration status, needs some way to receive health care should they need it, in the place where they are now. For this reason, as Linton and co-authors write:
Health care settings have historically been considered protected areas (also known as “sensitive locations”), where immigration enforcement was generally prohibited. Although rare examples of immigration enforcement had occurred in health care institutions, these were exceptions to historic enforcement practices. However, on January 20, 2025, the Trump administration rescinded the protected areas policy as part of a directive to expand immigration enforcement . . . This ambiguous and expanded reach of law enforcement creates confusion and anxiety among health systems and patients and is expected to have a chilling effect as immigrant families seek health care.
Given this policy change, leaders of health care institutions urgently need to update or develop practical guidance, grounded in ethical duties to patients and to health care workers, on how to respond to immigration enforcement encounters.
The framework below outlines three foundational ethical duties of health care institutions that can be enacted by leaders through policies, processes, and communication with their workforce: (1) the duty to plan for foreseeable situations with impact on patient care and institutional operations, (2) the duty to safeguard patient populations and the health care workforce, and (3) the duty of care, long understood as nonabandonment of patients.
The Duty to Plan
The duty to plan for emergencies that threaten public health and safety, such as infectious disease outbreaks, fires, extreme weather, and active shooters, also applies to situations that put a particular population at greater risk. Health care institutions should have predetermined responses for how staff should respond if immigration enforcement authorities enter their premises to obtain protected health information or remove patients, family caregivers, or health care workers.
Key features of the duty to plan for encounters with immigration enforcement in health care institutions:
- Establish lines of responsibility for interactions with authorities that ensure a point person for every shift.
- Institute a “front door” policy, procedure, and training that details and reinforces how security officers and other staff should interact with immigration enforcement authorities.
- Restrict access of immigration enforcement authorities to public spaces to minimize disruption to patient care. As much as feasible, identify and clearly label private spaces for patients, family, and health care staff only.
- Limit cooperation to what is required by law and require proper identification and appropriate legal documents before complying.
- Ensure protection and confidentiality of patient information, including through guidance concerning whether and how medically relevant information concerning immigration status (if known) should be reflected in electronic medical records.
The Duty to Safeguard
Health care institutions have a basic duty to safeguard their patients from harm, reflected in patient safety protocols. Safeguarding patients in the context of law enforcement is a familiar challenge for health care institutions providing care to patients in law enforcement custody. In those situations, health care workers need policies, procedures, training, and support for managing situations in which prison officials seek to assert authority over medical care or to obtain sensitive health information. Preparing health care workers for the possibility of interactions with immigration authorities should follow from the duty to plan and aim to prevent situations in which health care workers are unsure where they can turn for immediate guidance.
It is not ethically appropriate to leave the definition, practice, or responsibility of safeguarding patients up to individual health care workers. Ethical opinions differ about compliance with laws or policies that individuals may perceive as unjust. However, lack of institutional clarity concerning the basic duty to safeguard patients from harm can itself be a source of harm or injustice. Lacking institutional guidance, some workers may feel justified in taking unilateral actions (such as falsifying records) if they perceive that these actions are needed to safeguard immigrant patients; these actions may introduce inaccurate information into patient care systems. Other workers may feel equally justified in ignoring their duty to safeguard these patients. Reinforcing that the duty of care (see below) is foundational to health care work; it is owed to all patients and is integral to planning and to safeguarding.
Health care institutions are major employers, and immigrants are a significant percentage of health care workers at all levels. During heightened scrutiny of immigration status, safeguarding the health care workforce is also important. Institutional, departmental, and unit-level leaders should be attentive to how uncertainty and stress may affect the workforce, ranging from concern about one’s own safety or that of family members to disparaging remarks about immigrants or whether they deserve health care. These leaders should, through their own communication and conduct, set the tone for a collective commitment to the mission of patient care while acknowledging how the inherent stresses of health care work may be heightened by immigration enforcement.
Key features of the duty to safeguard in the context of encounters with immigration enforcement in health care institutions:
- Make trustworthy information available to patients, family caregivers, and the health care workforce.
- Partner with the National Center for Medical-Legal Partnership or other health law organizations and with knowledgeable staff such as medical social workers to provide expert training on topics relevant to the care of immigrant patients and family caregivers, including situations in which patients or caregivers face deportation proceedings.
- Ensure that patient care workforce training includes topics such as access to license in-person or remote medical interpreters.
- Provide opportunities for health care workers to reflect on their experiences and concerns in caring for immigrant patients.
- Recognize the chilling effect of immigration enforcement on health care utilization and, when possible, offer alternatives to in-person care such as phone or telehealth consultations.
The Duty of Care
This duty, often defined as nonabandonment, is foundational to ethical practice in health care. To faithfully care for patients is the core of health care professional identity. Being prevented from fulfilling the duty of care feels profoundly wrong. Health care institutions should support professionals’ ability to practice to standards of care and provide guidance and support for situations in which working to standards is undermined by factors such as insurance or immigration status. Institutions should also strive to uphold their duty of care to the neighborhoods, cities, or regions where they serve as health care providers and as employers.
Health care workers in patient care roles often think of themselves as advocates for patients and their families. This identification may be especially strong when patients’ access to needed care is constrained, and yet there are limits on how much a health care worker can or should be expected to do for any patient or family in their professional role. The duty of care owed to all patients does not require individual workers to assume responsibility for all forms of advocacy that may be needed, nor to extend themselves without limit. Institutional recognition of barriers to care and institutional support for programs to reduce access problems associated with immigration status are fairer and more sustainable than unofficial systems of advocacy dependent on individuals.
Fears about legal consequences can undermine the duty of care. Under conditions of uncertainty and stress, it is crucial for institutions, through departmental and unit-level leaders, to respond to workers’ questions and concerns about liability, reinforce obligations to patients that include safeguarding their privacy and the confidentiality of health information, and clarify where health care workers should turn when they need guidance.
The key features of the duties to plan and to safeguard, described above, support the duty of care. Specific key features of the duty of care in the context of immigration enforcement in health care institutions:
- Foster a welcoming and caring clinical environment that respects all patients.
- Maintain clarity concerning appropriate standards of care for emergency and nonemergency medical treatment for all patients; do not compromise those standards if an avenue to meet them exists.
- When standards of care cannot be met for some patients because of immigration status or immigration enforcement actions, maintain responsibility for their care and pursue the least harmful approach to responding to their needs. Clinical ethics consultation may be helpful.
By applying this ethical framework, health care institutions can navigate foreseeable uncertainty and support the safety, health, and well-being of patients, caregivers, and the health care workforce.
Sabrina Derrington, MD, MA, HEC-C, is director of the Center for Pediatric Bioethics at Children’s Hospital Los Angeles and an associate professor of clinical pediatrics at Keck School of Medicine of USC.
Nancy Berlinger, PhD, MDiv, is a senior research scholar at The Hastings Center.
Lynette Martins, LL.B, PGDip, MBE, LL.M, will be the Jaharis Faculty Fellow in Health Law and Intellectual Property at DePaul College of Law in fall 2025. @Lynettemartins.bsky.social
Rachel Fabi, PhD, HEC-C, is an associate professor of bioethics and humanities at SUNY Upstate Medical University. @fabioethics.bsky.social
Laura Guidry-Grimes, PhD, HEC-C, is an associate staff ethicist and a clinical assistant professor at the Cleveland Clinic Lerner College of Medicine.
Amelia Barwise, PhD, MB, BCh, BAO, is associate professor of bioethics and of medicine at the Mayo Clinic in Rochester, Minn.